Enabling better healthcare management
Create® Technology elevates your health plan and administration
People are using technology to manage virtually every aspect of their lives – from banking to shopping to ordering food and rides. Now, Brighton Health Plan Solutions has developed healthcare technology to simplify health plan management.

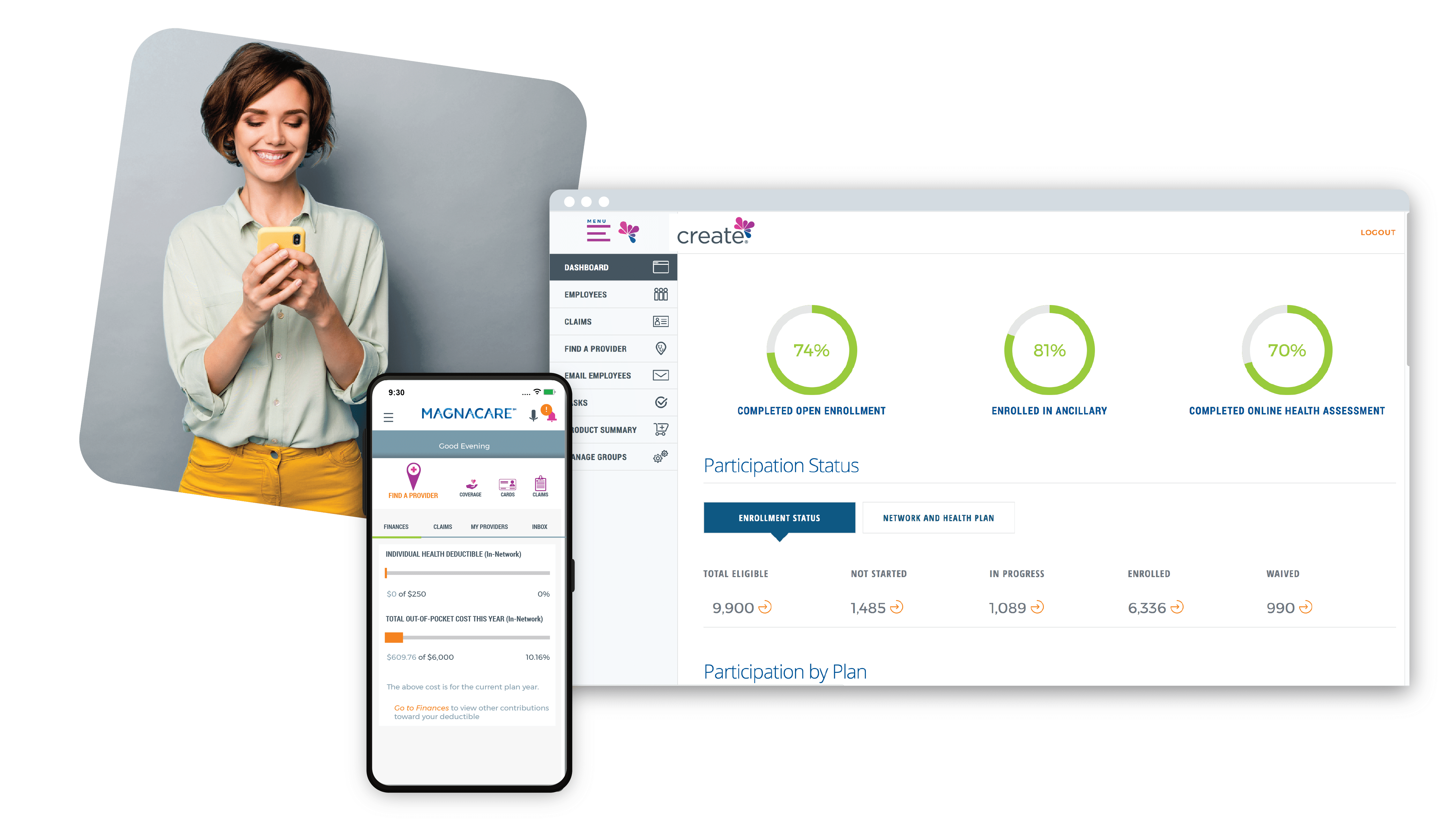
Our award-winning, innovative Create® Technology platform enables all aspects of health plan access, including tools for online open enrollment, benefits administration, and member activation and engagement. It integrates with our MagnaCare health plans and integrated delivery network (IDN) health plans, as well as with any other health plan on the market.
Create® Technology integrates with third-party vendors to provide a one-stop shop for managing medical and ancillary benefits. The platform also handles healthcare enrollment and eligibility according to your criteria, as well as payroll administration.
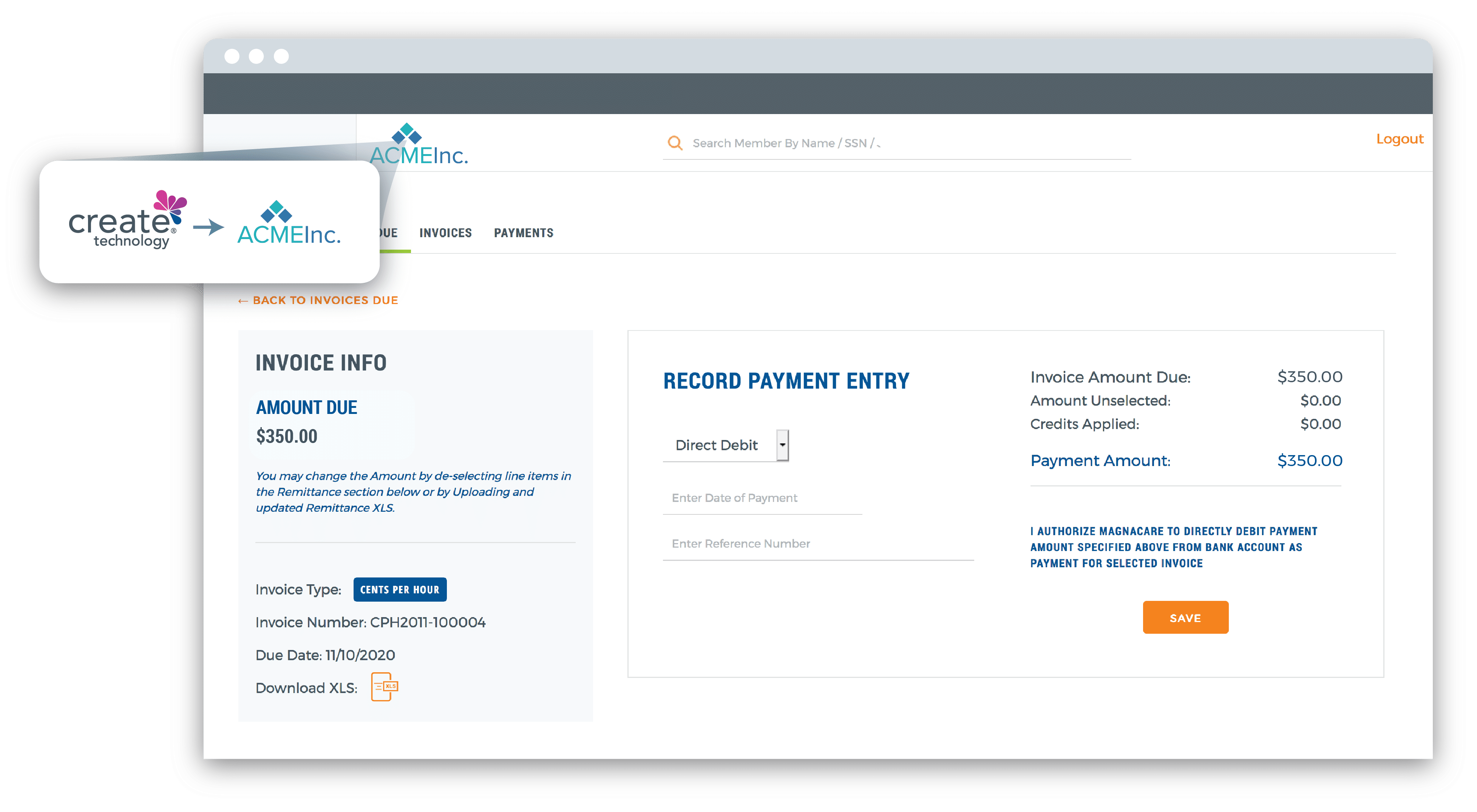
We’ll customize the flexible platform with your logo, rules, and processes – enabling you to quickly roll out a technology solution built by experts in health plan and benefits management.
Who uses the Create® Technology platform?
Our industry-leading healthcare technology platform is highly sought-after in the marketplace, used by all stakeholders:
- Benefits managers – to manage the health plan and give plan members easy access to their benefits
- TPAs – to manage their clients’ claims and offer advanced technology to their clients
- Health systems who offer their own health plans – to manage their health plans and to give online access to their clients and members
- Members – to gain 24/7 access to the member portal and mobile app, where they can find providers, review their benefits, display their ID card, check EOBs and finances, and more
What you will gain
Simplify health plan management
Never forget a task
Manage eligibility and enrollment
Easily update member status, add dependents, and so on, and automatically update the member on account changes. Our system automates the process of tracking hours, monthly payments, and other eligibility criteria, identifying employees who are newly eligible or no longer eligible for coverage.
Manage claims
Review and/or process claims and look for high-dollar amounts. Member privacy is protected because sensitive Private Health Information (PHI) is blocked in the employer view.
Generate reports
Create actionable reports on claims and financial information, based on the criteria you select.
Centralize HR administration

Increase member engagement
Members access information quickly and easily
Members use the online member portal to find providers, view their claims and EOBs, check their medical and ancillary benefits, and more.
Quick contacts
In one click, members can call, chat, request a callback or email customer service.
On-the-go access
The intuitive mobile app provides members with all the online functionality, wherever life and work takes them. And, as long as they have their phone, members will always have their ID card.
Educate members about their benefits
As members become more involved with their healthcare, they make better healthcare choices. Our technology makes your members wiser, more efficient users of healthcare.
Effectively communicate without the high cost
The Create® Technology platform eliminates slow, costly mailings. You can instantly contact all members or only a specific group, based on criteria selected. Send out any type of communication, customized to your needs, such as announcing an emergency situation or an important meeting. Automated notifications alert members based on actions taken by the member or administrator.
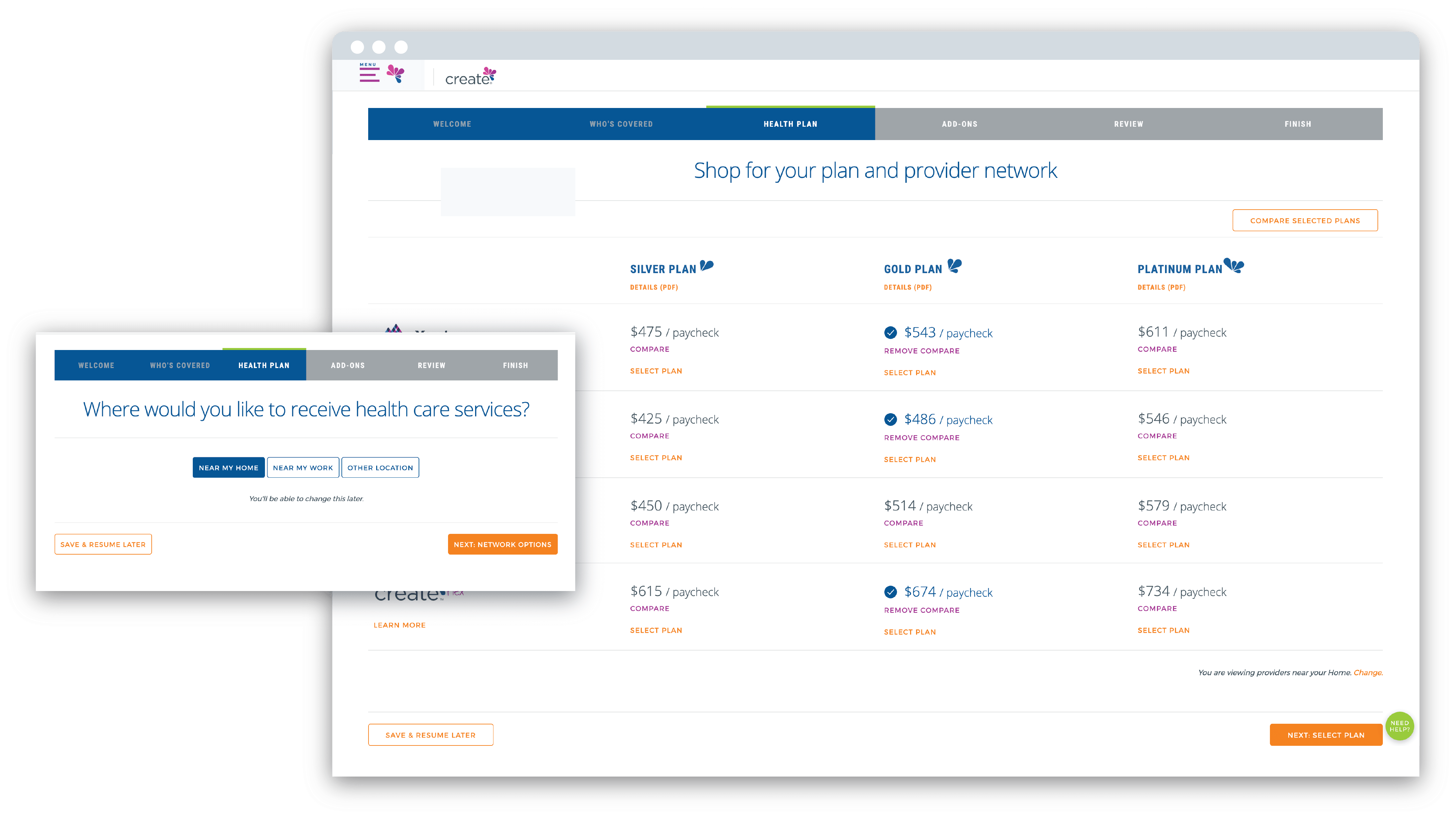
Eliminate manual enrollment
Receive all required
information the first time
The enrollment tool leads members through the process, ensuring all information is correct and complete. Our system even prompts the enrollee for required documents, such as birth certificates for dependents.
Reduce your team’s effort
Go live faster
With all information already verified and online, you reduce your team’s post-enrollment work, which shortens the time to go-live.
Re-use data year after year