54% of patients say maximum acceptable wait time for an appointment is two days, according to new survey
For patients, “convenience” in healthcare means minutes saved, and care that fits into already busy lives. According to recent data, that convenience is disappearing. National tracking from AMN Healthcare puts average appointment wait times in large metropolitan areas at 31 days — the highest since the organization started tracking the metric. That means the reality for most people needing care isn’t deciding between “Who’s best?” but “Who’s available?” And these decisions are almost always determined by insurance. Most people aren’t shopping in an open market; they’re choosing from a limited number of in-network options.
These waits are extending at a time when American consumer culture is becoming accustomed to instant gratification. Whether it’s in travel, retail, or finance, most industries default to immediate confirmations. By comparison, scheduling in-network healthcare almost always involves playing phone tag, feeling unclear about next steps, or being forced by automated systems to restart the booking process, adding time and effort.
Against that backdrop, Brighton Health Plan Solutions surveyed 600 U.S. adults (18+) in September 2025 via third-party platform Pollfish to learn how they define convenience in healthcare. The answer was clear: Convenience is the shortest path from intent to a confirmed visit. Same- or next-day availability and instant online booking now rival, and sometimes outweigh, traditional factors like number of choices. When systems make that path obvious, patients stay in-network and will even accept fewer options to get faster appointments.
As wait times grow and insurance choices narrow, patients are picking the fastest route to care. That often means urgent care is used when immediacy is most important or virtual visits are chosen to meet certain clear and timely use cases. These options become pressure-release valves when primary care can’t fully meet patients’ needs.
“The message is simple: convenience builds trust,” said Michelle Zettergren, Chief Sales and Marketing Officer with Brighton Health Plan Solutions. “Clear timing, easy access, and good communication builds trust before the visit even begins. As healthcare becomes more transparent, those experiences will stand out even more.”
What patients really want is certainty. Give them a time, a straight answer, and a clear bill, and they’ll come back. Policy is already moving us in that direction with clearer rules on sharing information, pricing, and prior authorization. Telehealth policy will shape what at-home access looks like next. The survey results back this up: When speed is guaranteed and booking is easy, patients remain loyal. That promise shows up as real-time scheduling, some after-hours capacity, and plain-English communication.
Executive Summary
- Primary Care Provider Loyalty Remains: Nearly nine in 10 patients (89%) would choose their primary care provider (PCP) over urgent care if same‑day appointments were guaranteed.
- Online Booking Matters: Six in 10 patients (60%) say the ability to book online instantly is extremely or very important when choosing a provider.
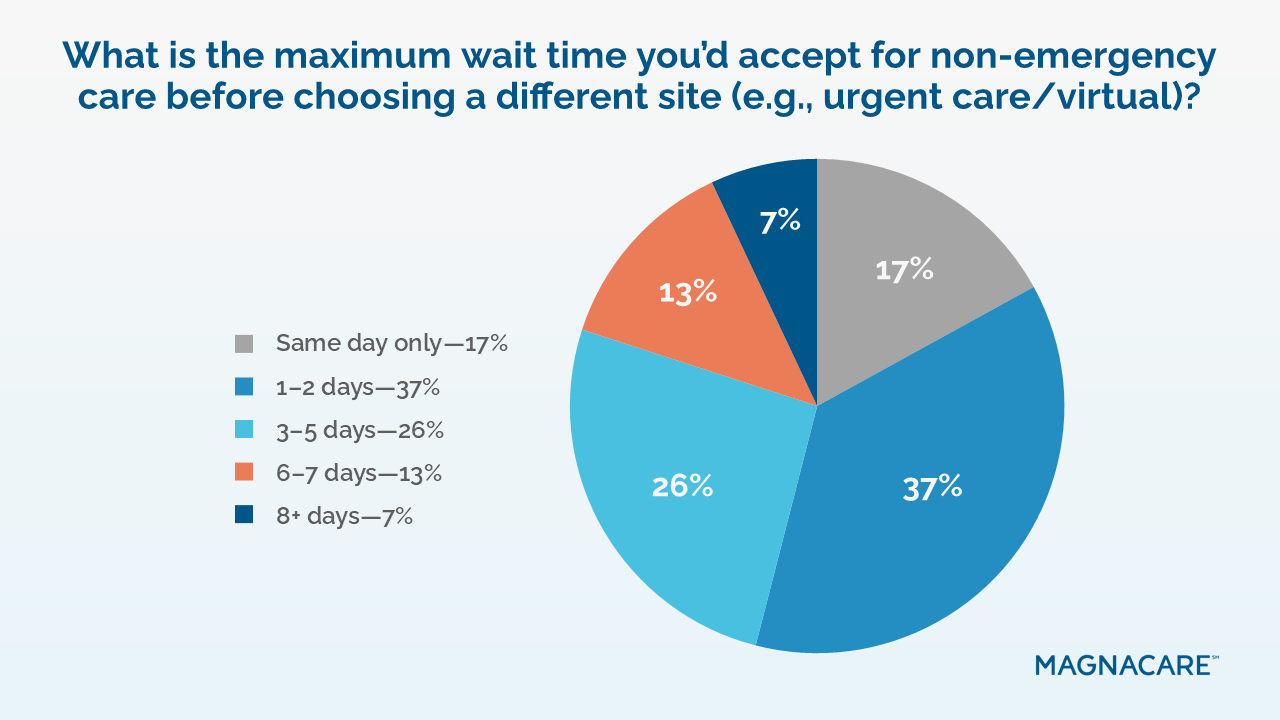
- Short Wait Times Expected: More than a third of patients (37%) say an acceptable wait time for routine visits is just one or two days, while 17% say only same-day access is acceptable.
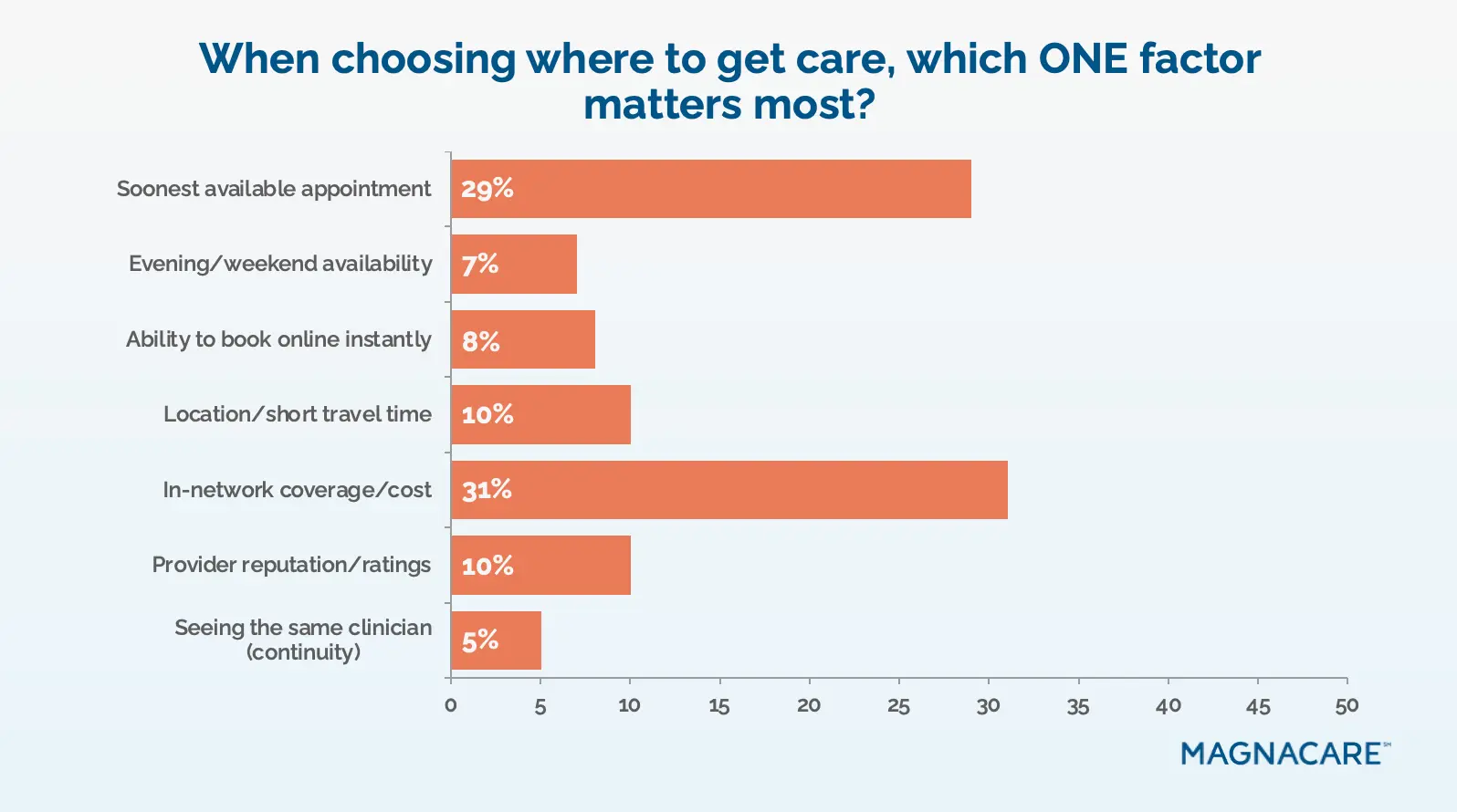
- Cost vs. Access: 31% pick in‑network cost and coverage as the top decision factor, while 29% choose whichever provider has the soonest available appointment.
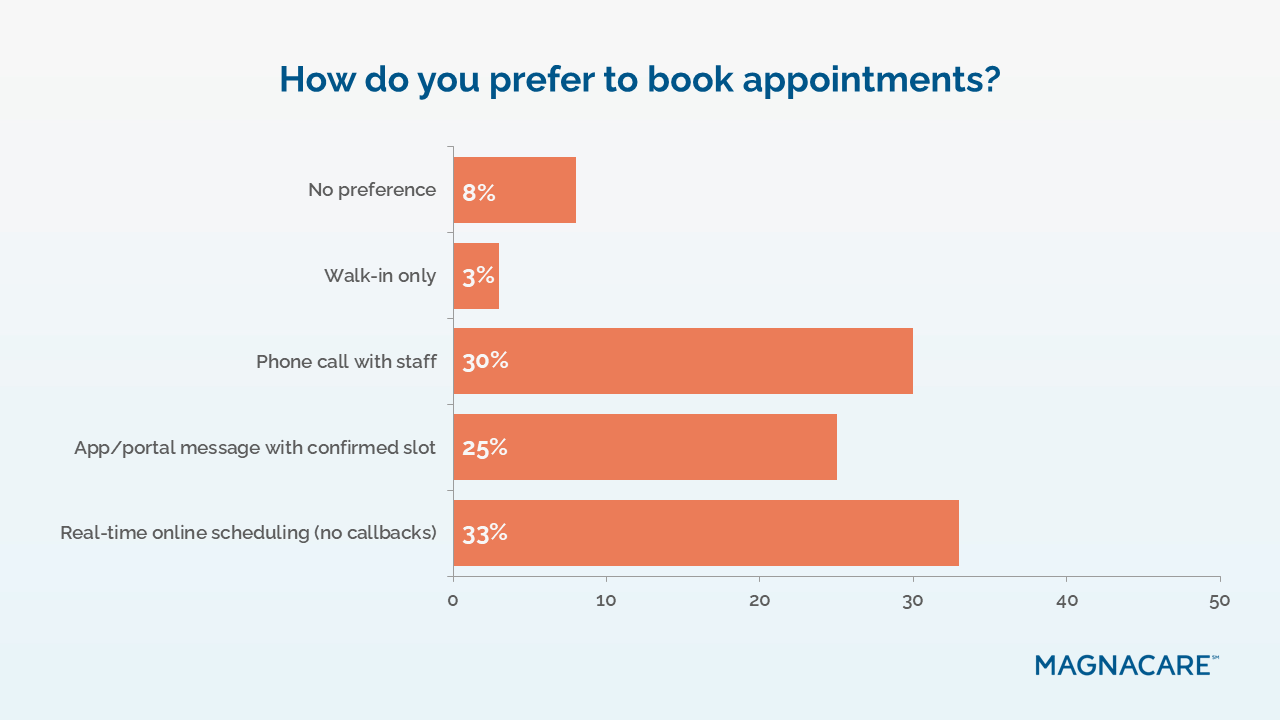
- Scheduling Shifts Online: One-third of patients (33%) prefer real‑time online scheduling, compared to 30% who favor phone calls and 25% who use portal messages.
- Same-Day Access Gaps: Only 43% say they “always” or “most of the time” get a same-day appointment when they want one, while nearly a quarter (24%) say they never do.
- Choice Sacrificed for Speed: More than half of patients (51%) would accept fewer doctor or hospital choices if it meant they could get much faster appointments.
- Employer Options Appeal: Nearly three-quarters (74%) are likely to use an employer‑offered local doctor or hospital option that functions like an in‑network plan.
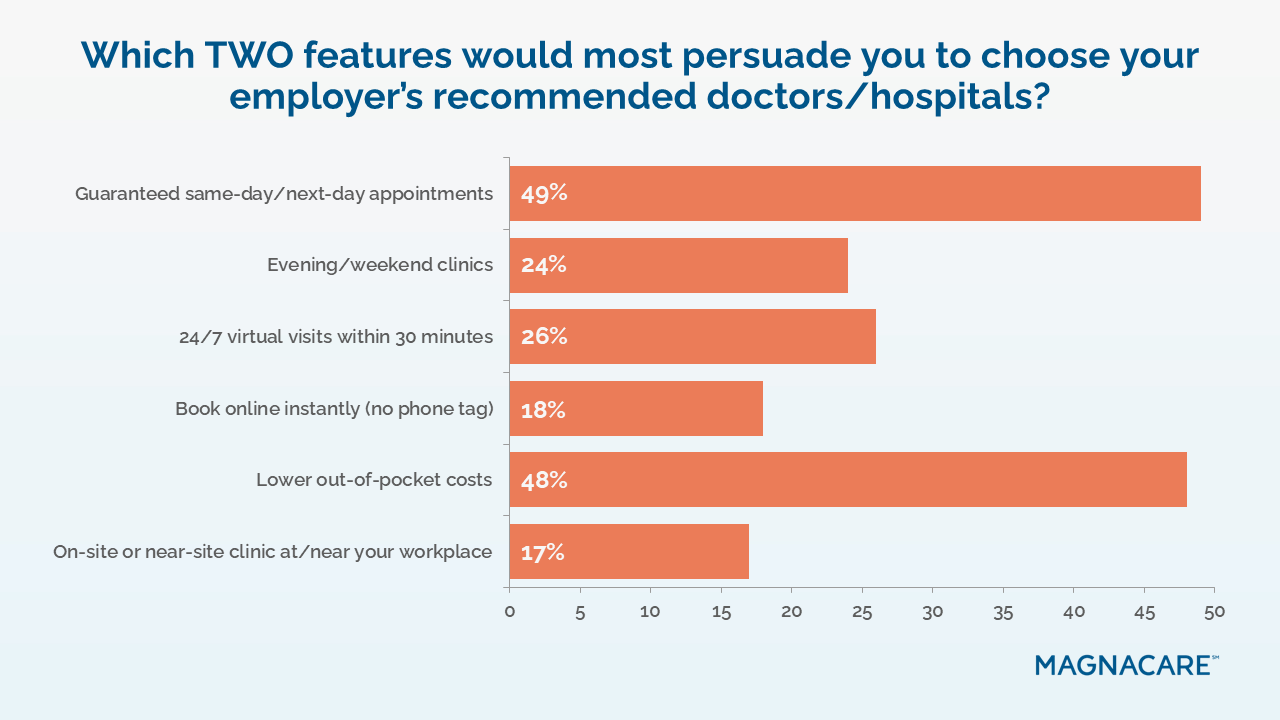
- Persuasion Factors Differ: Guaranteed same- or next‑day appointments would persuade 27% to choose employer‑recommended providers, while 26% say lower out-of-pocket costs would do the same.
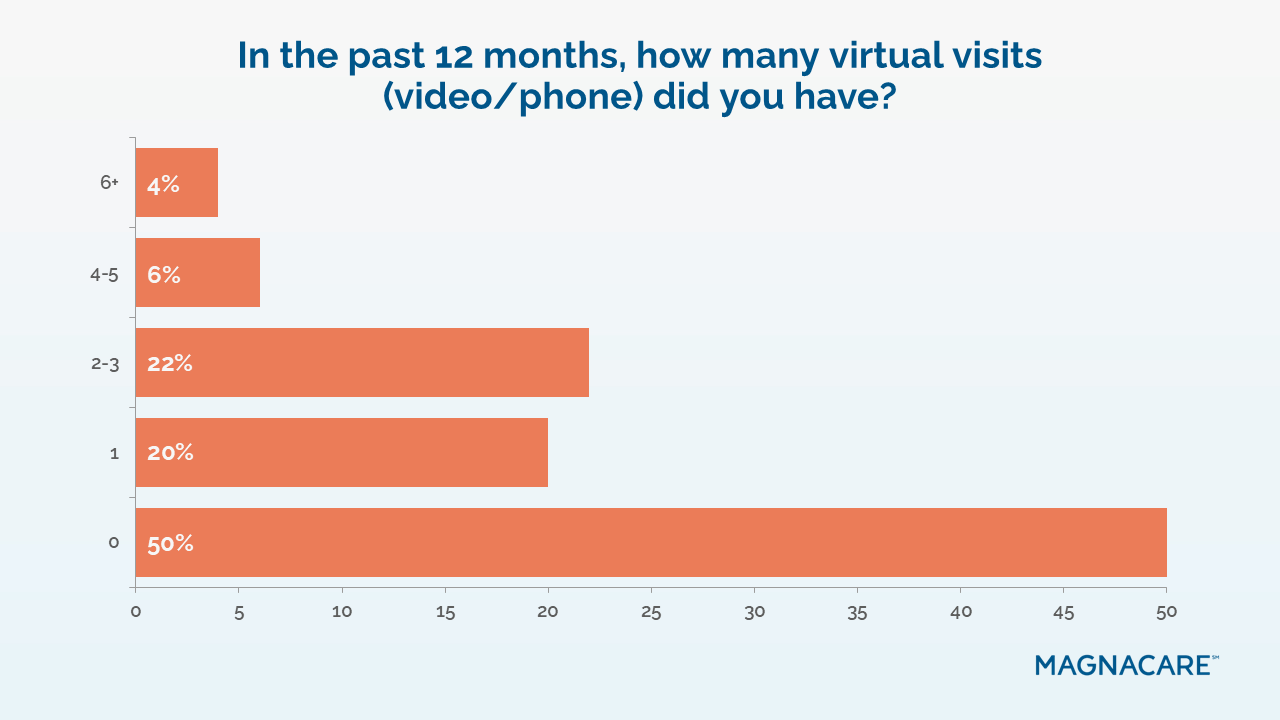
- Virtual Care Unused: Half of patients (50%) report having no virtual visits over the past year, even though time savings (36%) and faster access (27%) are their top reasons for considering virtual care.
“Fast access” defines convenience — and expectations are tight
Patients are telling us that convenience is mostly about time. In their mental model, “good access” means seeing someone quickly without jumping through hoops. That’s why “soonest available appointment” is nearly equal to “in-network cost/coverage” as the top decision driver — 29% versus 31% — and why so many define convenience through “same-/next-day options” (62%). It’s a recalibration of expectations shaped by the rest of consumers’ lives: certainty now, not callbacks later.
The practical line in the sand is 48 hours for routine care. More than one third of respondents cap an acceptable wait at 1–2 days (37%), with another group insisting on same-day appointments (17%). The conclusion is straightforward: in this market, time is trust.
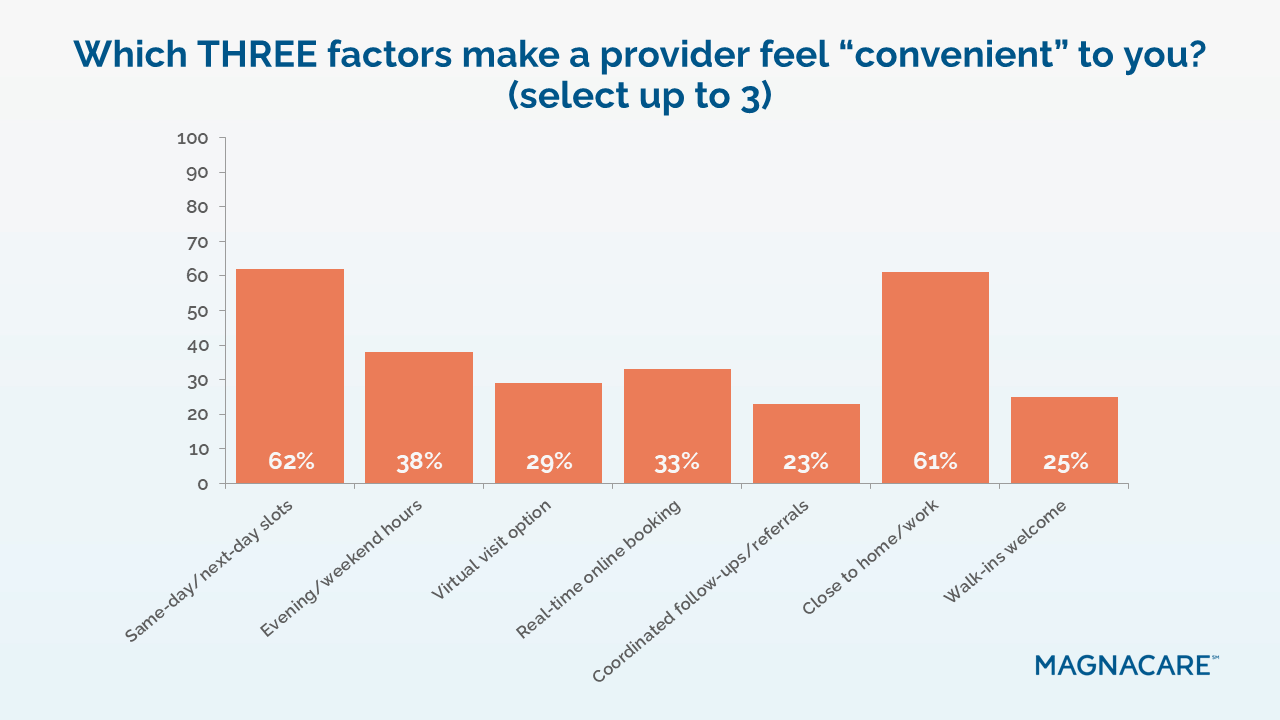
For health systems, make the promise of same- or next-day appointments obvious and real. Show open slots, confirm in the moment, keep some evening and weekend availability in the mix, and showcase times plainly online and in the app.
For large employers or self-funded plans, make speed part of the deal, not an afterthought. Point people to providers who can see them today or tomorrow, and put those booking links where employees already are. Simpler path, faster visit — that’s what keeps them using the network.
Guaranteed same-day would pull patients back to primary care
Urgent care thrives because it reliably reduces delays in care. But the data shows this advantage is conditional. If primary care could match that speed, patients would prefer continuity with their personal clinician. In fact, nearly all surveyed (89%) would choose their PCP over urgent care given a same-day guarantee. Today, however, less than half (43%) say they usually get same-day when they want it, and less than a quarter (24%) say they never do. That gap, more than preference, explains the uptick in urgent care usage.
This reveals that leakage is a delay problem, not a loyalty problem. In the era of instant gratification, patients aren’t walking away from primary care as a concept; they’re walking toward whoever can see them now.
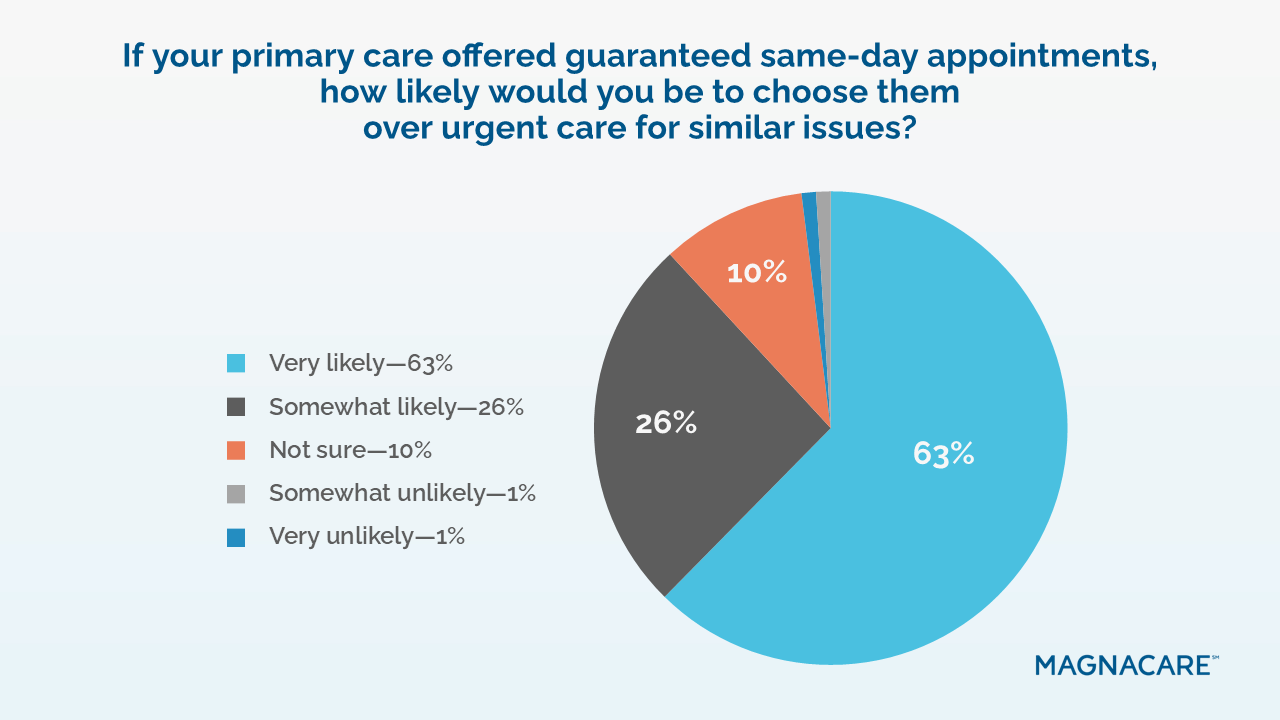

For health systems, a clearly communicated same-/next-day standard in primary care is a competitive tool for increasing domestic utilization and preventing fragmented care. For employers/self-funded plans, building navigation around explicit time guarantees keeps members in-network and out of higher-cost settings without asking them to sacrifice continuity.
Digital convenience (instant online booking) is now table stakes
The majority of respondents say instant online booking is extremely or very important (60%), and when forced to choose how to book, real-time self-scheduling (33%) beats calling staff (30%). In other words, the experience that wins is the one that confirms an appointment time in the same session.
The takeaway isn’t that digital tools and apps solve everything; it’s that digital is the mechanism that best delivers on quick and convenient care. And features like real-time scheduling and immediate confirmation are key to building patient trust.
For health systems, exposing live capacity across all platforms and retiring the “request an appointment” dead-end button turns need into confirmed, booked care. For employers or self-funded plans, requiring real-time scheduling integration in member tools ensures that employees appreciate the network’s access advantage.
Virtual care’s promise is underrealized: high interest, uneven use
Virtual visits remain underutilized for general care. Half of respondents report zero virtual visits in the last year (50%), even though they’re most comfortable using that method for clear, routine tasks, like medication refills or management. When people do choose virtual, their reasons are strikingly practical: no travel needed and time savings (36%) and faster consultations (27%). This signals that the demand exists, but patients need an obvious, credible pathway to use virtual care.
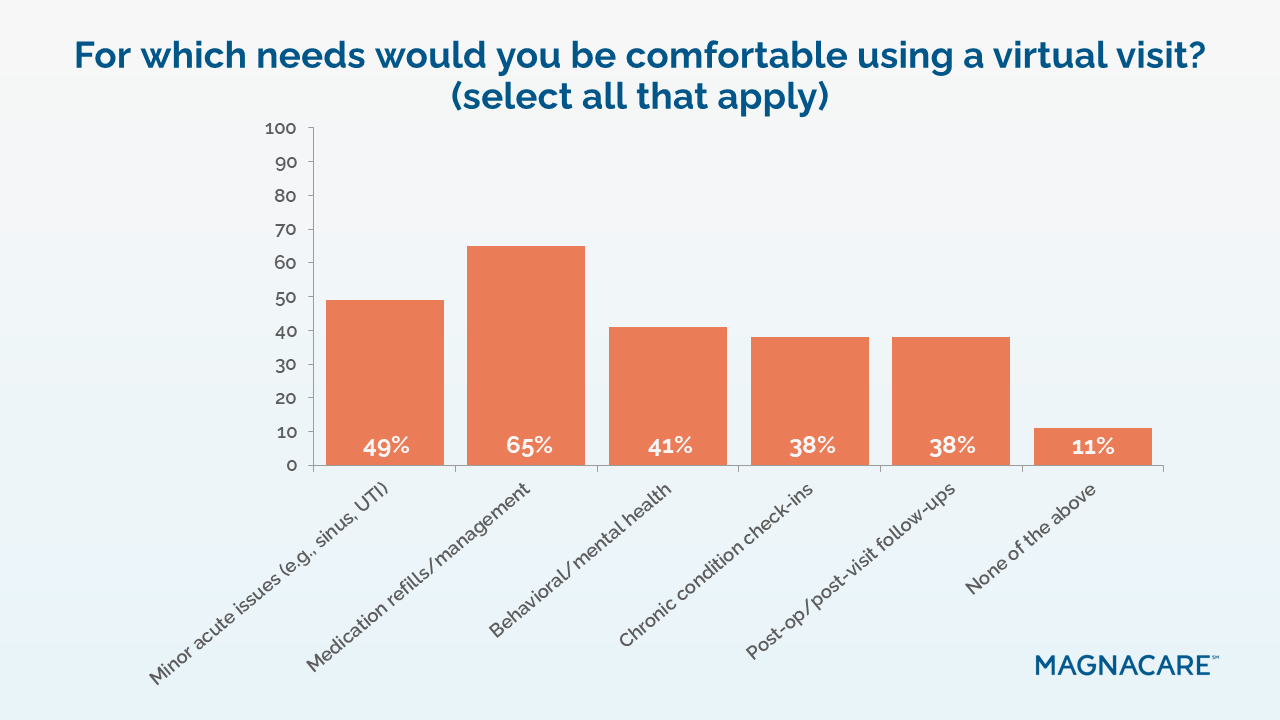

For health systems, it’s important to tell patients upfront which problems are easily solved by video, like medication refills, minor rashes, pink eye, prescription questions, or simple follow-ups. Then, make those options easy to find and select on homepages, apps, and phone menus. Give a clear response promise, like “video visit today” or “a clinician will reply within an hour.” If a video visit isn’t enough, book the in-person slot during the same interaction so no one has to call back. For employers or self-funded plans, promote virtual for the specific use cases employees already accept, so savings are captured and convenience they can feel is delivered.
Employers can steer with convenience — but must increase awareness
Members are open to employer-facilitated options when the value is obvious. A strong majority (74%) say they’re likely to use an employer-offered local option that functions like in-network. The nudges that move behavior are clear: guaranteed same- or next-day appointments (27%) and lower out-of-pocket costs (26%). Yet awareness is uneven. Thirty-eight percent aren’t familiar with these offerings, which means latent demand is leaving value on the table.
The conclusion is that employers are a valuable channel for convenient care, but only if it’s framed simply enough for members to act in the moment.
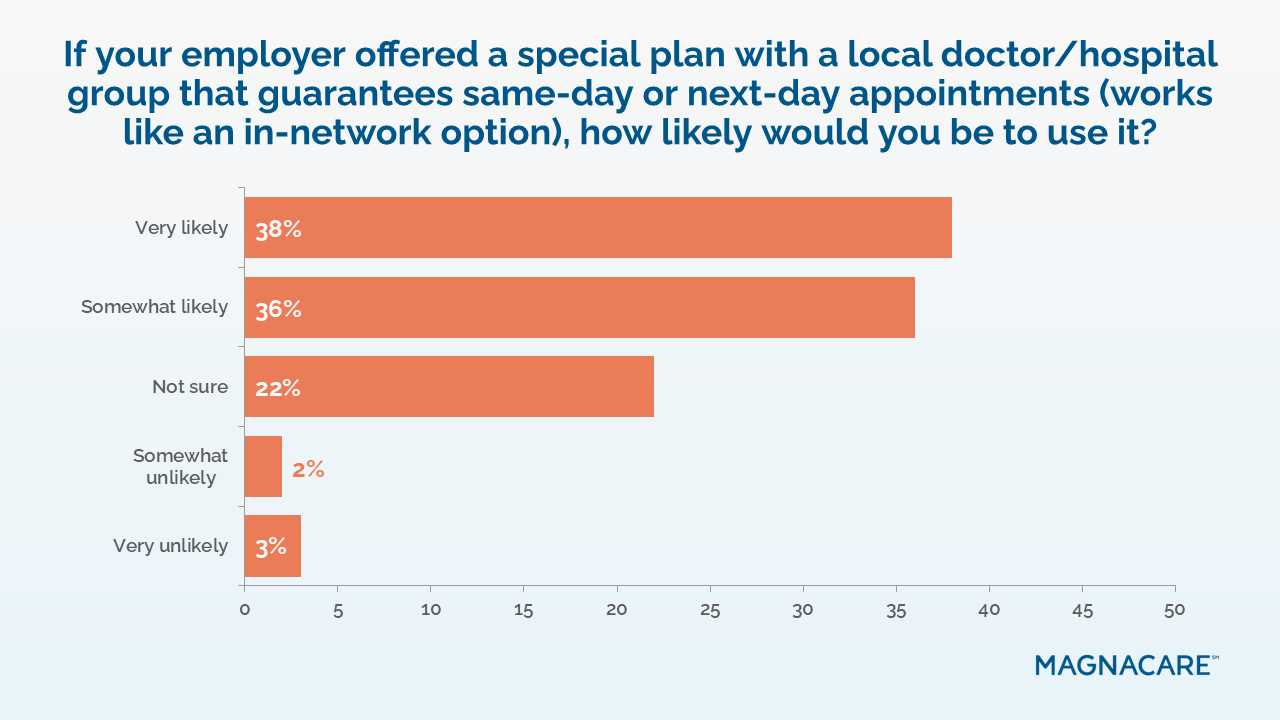

Health systems should therefore package employer partnerships as access bundles (time guarantees + instant booking + clear pricing) and report performance transparently. Employers or self-funded plans should put those guarantees and booking links in the places employees already go, like benefits portals, ID cards, and care-navigation apps, so the promise of convenience is only one tap away.
Next Steps: Making the Fast Path Obvious
For health systems hoping to serve a large employer or an employer exploring a deeper partnership, the shared opportunity is to make that path not only easy to see but also easy to integrate into the coverage people already have. What follows isn’t a rigid playbook, but a set of conversation starters that can be shaped to target markets.
Align on what “convenience” means
Start with a shared definition the employer and patient can both live with: convenience is the shortest path from “I need care” to a confirmed time. Prioritize convenience on the health system’s website, app, and call center, and the employer’s benefits portal and navigation tools. When looked at together, the sticking points show up fast: unclear choices, dead ends, or extra handoffs that cost people time.
Explore alternatives to the usual access model
Use the avenues already in place, like primary care, urgent care, and virtual care, in a way that brings the fastest appropriate option to the top. For a health system, that can mean letting simple issues start virtually so that same- or next-day office visits stay open for hands-on needs. For an employer, it means pointing employees to those options in one place, so they can pick a time, book it, and move on with their day.
Begin cross-functional discussions
Bring the people who shape the first steps of care into the same room: access and scheduling, clinic operations, digital tools, and patient experience. Sit alongside the employer’s benefits and communications leads. Use this report to walk through where patients get stuck now and which routine needs could move faster with small, coordinated changes.
Invite local partners into the conversation
If serving or employing a large local population, compare notes on a few plain signals: how soon routine care is available, how someone accesses care (click, call, or walk-in), and what video can handle. The goal isn’t to add more choices. It’s to make the right choice obvious inside the plan people already use. A short list of shared signals goes a long way.
Make performance more visible over time
Talk about access in simple terms and put that messaging where people will see it. Next available appointment windows and quick confirmations are easy to understand and even easier to trust.
Conclusion: Turning Convenience Into a System Promise
Patients read convenience as a promise: see me soon, make it simple, and keep me informed. In these survey findings, the details vary, but the story is the same: people choose the care that best respects their time. Same‑ or next‑day slots, clear booking, and straightforward communication shape trust before anyone walks through a door. In that sense, convenience is not an add‑on to quality; it’s how quality is first experienced.
“These numbers show that time is the new measure of trust in healthcare,” said Zettergren. “People don’t want to hunt for a timeslot; they want a quick answer and a near-term appointment. When the process is that simple and clear, people will come back and remember their experience for the right reasons.”
For health systems and large employers exploring deeper partnerships, this is the common language. When the path to timely appointments is quick and easy, patients stay, follow through, and remember the experience for the right reasons. Convenience is how trust is built, and it’s how care begins.

